INTRODUCTION
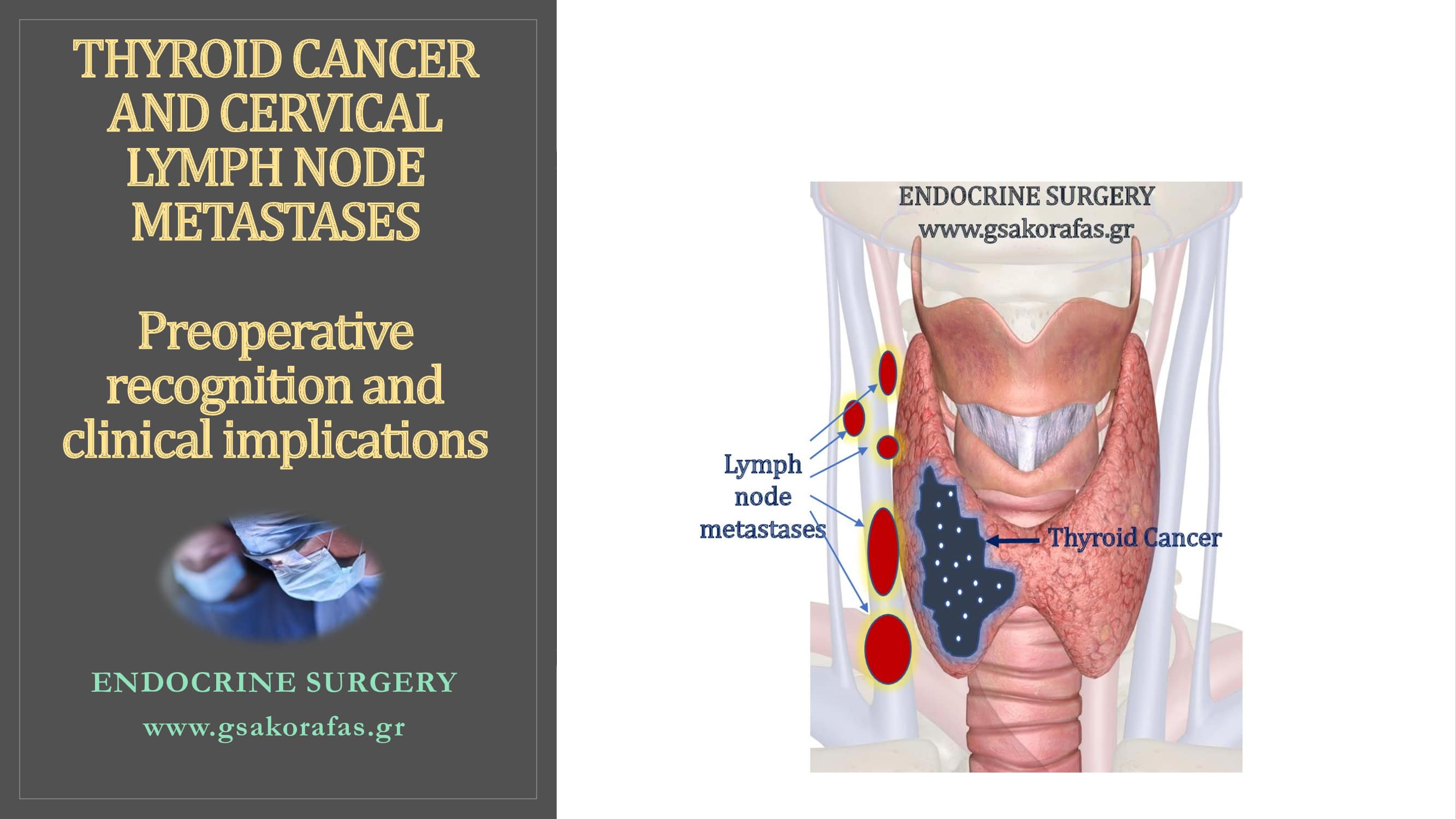
Thyroid cancer frequently metastasizes to cervical lymph nodes. It has been estimated that cervical lymph node metastases are present in 20 – 50 % of patients with differentiated thyroid cancer. This percentage is even higher in patients with medullary thyroid cancer. Lymphatic spread is possible even in small and totally intrathyroidal thyroid cancers. Of note, micrometastases (defined as maximum diameter of less than 2 mm) may be present in up to 90 % of patients.
METHODS FOR PREPERATIVE IDENTIFICATION OF PATHOLOGIC CERVIVAL LYMPH NODES
Modern imaging allows accurate preoperative staging of thyroid cancer.
Neck ultrasonography
Detailed neck ultrasonographic examination identifies involved or suspicious cervical lymph nodes in a significant percentage of patients (up to 40 %). This information alters surgical approach in up to 20 % of patients.
Ultrasonographic evaluation should include both central and lateral neck lymph nodes and be performed when cytology signifies the presence of thyroid cancer or raises suspicion for malignancy. The experienced radiologist provides the surgeon a detailed lymphatic mapping, which is of paramount importance in planning and executing lymph node dissection.
Fine-Needle Aspiration
Ultrasound-guided fine-needle aspiration (FNA) cytology should be performed for sonographically abnormal nodes > 8 – 10 mm. However, the possibility of false-negative results should be kept in mind.
The addition of measurement of thyroglobulin (Tg) levels in the aspirate (wash-out) may increase diagnostic accuracy, especially when the lymph node is cystic (cytology is often inadequate in these cases)
Cross-sectional imaging
Ultrasonography is the preferred imaging method in the preoperative evaluation of the patient with thyroid cancer. Computed tomography is not routinely indicated in these patients.
However, computed tomography could be useful in some selected cases, such as:
- extensive nodal involvement in the neck. These patients may have nodal disease in other areas beyond the neck visible by ultrasonography (see below)
- nodular disease in the mediastinal, infraclavicular, retropharyngeal, and parapharyngeal spaces
- nodular disease extending within muscles, vasculature and/or upper aerodigestive organs
Magnetic resonance imaging / Positron Emission Tomography (PET)
Sensitivities of these modern imaging methods for the detection of cervical lymph node metastases are low (30- 40 %). These expensive methods should not routinely used for the preoperative staging of patients with thyroid cancer.
CLINICAL CONSIDERATIONS
This very high incidence of cervical lymph node metastases in thyroid cancer explain why metastatic lymph nodes represent the commonest site of persistent/ recurrent disease.
Accurate preoperative recognition of involved cervical lymph nodes is of paramount importance for the planning of the appropriate surgery. Obviously, total thyroidectomy is inadequate in patients with PTC and lymphatic spread of the disease. In these patients, lymph node dissection should be performed concomitantly with thyroidectomy. Moreover, accurate preoperative evaluation of the EXTENT of lymphatic spread allows the selection of the optimal EXTENT of lymph node dissection.
Failure to identify pathologic or suspicious lymph nodes during preoperative evaluation typically result in a suboptimal surgical treatment. Incomplete surgery may complicate further (adjuvant) treatment, including radioactive iodine ablation. Further surgery may be required to achieve radical resection of the disease. However, reoperations are typically more difficult, due to the presence of fibrotic tissue in the operative field, due to previous surgery. In addition to increased technical difficulty, reoperations are associated with increased morbidity. This emphasizes the importance of radical and curative tumor resection during initial surgery.