Introduction
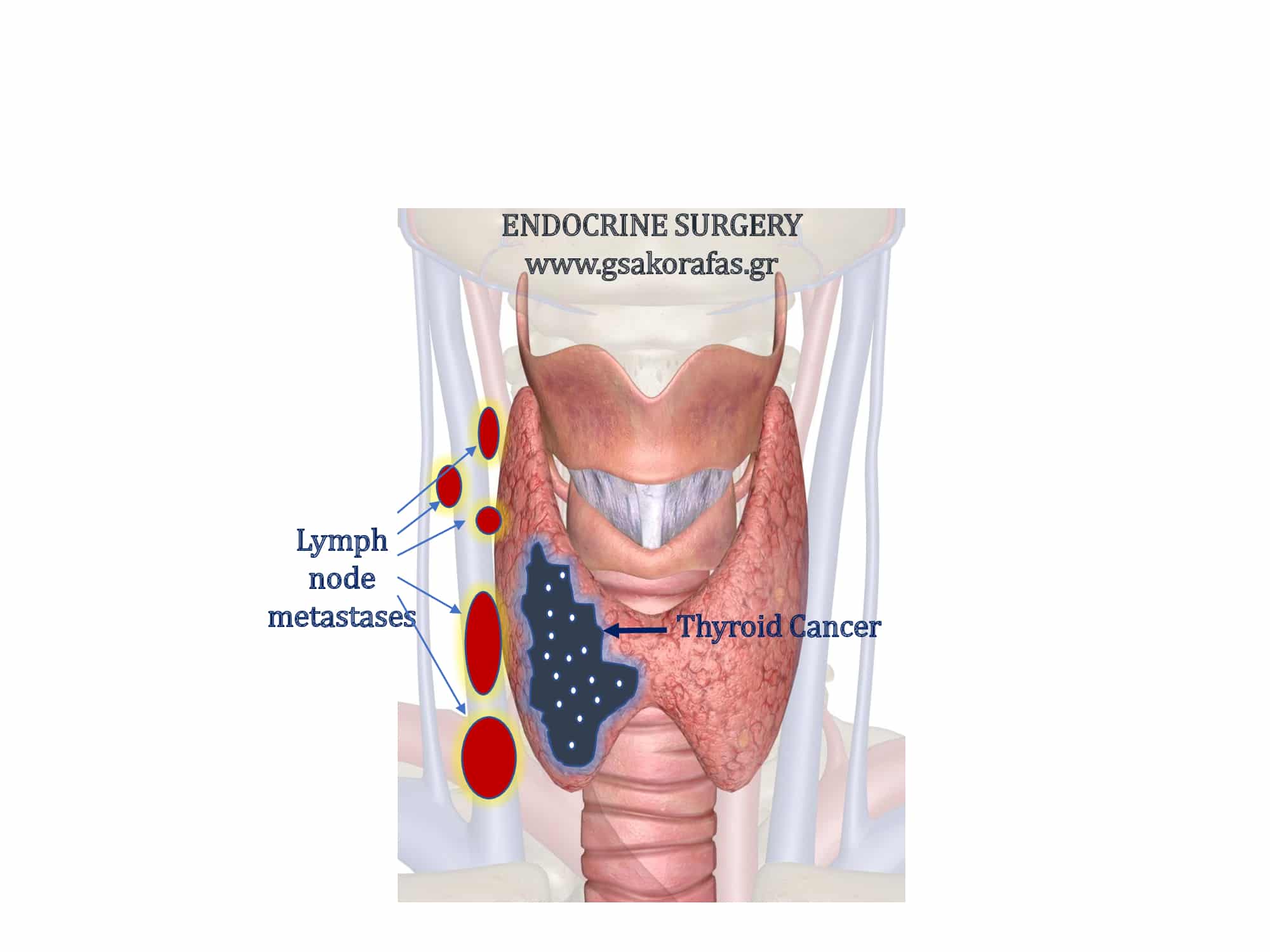
Lymph node metastases are very common in patients with papillary thyroid cancer. However, all these metastases are not the same in terms of their implications for recurrence and mortality.
Macrometastatic vs. micrometastatic disease
Macrometastatic disease is defined as the presence of lymph node metastases detected clinically or based on results of preoperative imaging or intraoperative findings. In contrast, micrometastatic disease is detected following histopathological examination of resected lymph nodes.
Macrometastatic lymph node disease in papillary thyroid cancer is associated with higher recurrence rates and potentially with increased mortality. This association is observed especially in patients who are 45 years or older or when metastases are large (> 3 cm). By contrast, microscopic lymph node metastases do not affect patient survival and are associated with much lower rates of recurrence.
Nodal volume and prognosis
The ATA (American Thyroid Association) published a detailed systemic review, quantifying the relationship between nodal volume and its relationship to prognosis in thyroid cancer. It has recommended that patients be classified into ‘lower’ and ‘higher’ risk N1 categories, based on number and size of nodal disease. “Low-risk N1” was defined as ≤ 5 positive lymph nodes measuring ≤ 0.2 cm in maximum diameter. Patients with ‘low-risk N1’ papillary thyroid cancer are generally considered in the same low-risk for recurrence category as N0 patients. In contrast, higher risk is associated with
- > 5 positive lymph nodes
- large node size
- extralymphadenic extension
- high ration of involved / total resected lymph nodes
[/vc_column_text][/vc_column]